Pelvic Health Awareness Month: Why Pelvic Health Matters to Women
Understanding Pelvic Pain: Causes, Diagnosis, and Comprehensive Treatment
Introduction: Navigating the Complexities of Pelvic Pain
Pelvic pain, a common issue faced by women, can arise from various causes. This comprehensive guide aims to explore the intricacies of pelvic pain, from its potential origins to the sophisticated diagnostic methods and personalized treatment options, with a focus on Dr. Hema Jonnalagadda's expert approach at Advocare Montgomery Gynecology.
Understanding the Causes of Pelvic Pain
Pelvic pain is a multifaceted issue with various underlying causes, each requiring a unique approach to diagnosis and treatment. Dr. Hema Jonnalagadda at Advocare Montgomery Gynecology specializes in identifying and treating these diverse causes with a patient-centric approach

Menstrual Cramps (Dysmenorrhea)
● Overview: A common cause of pelvic pain, dysmenorrhea is characterized by cramping or throbbing pain in the lower abdomen, typically linked to the menstrual cycle.
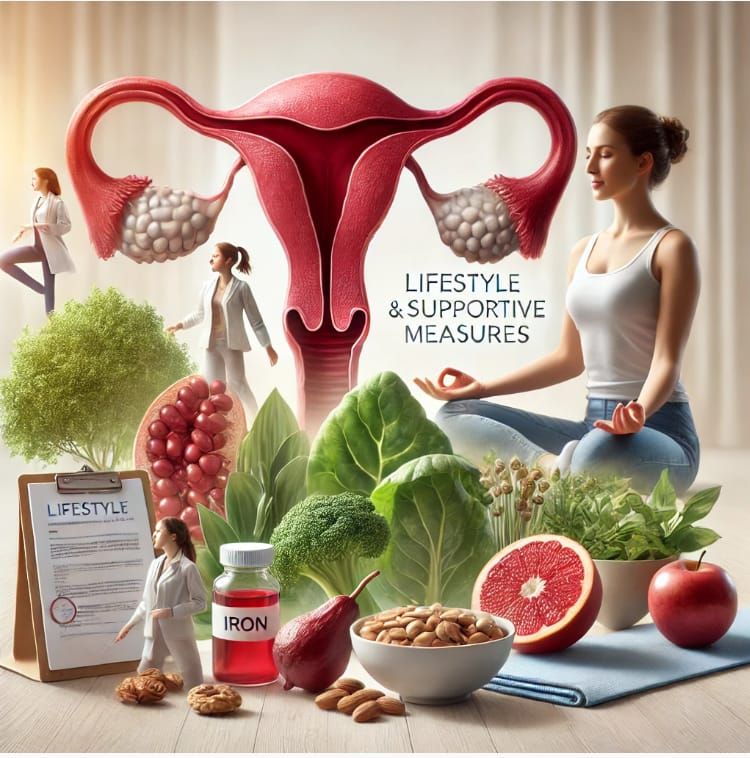
● Management: Treatment often includes nonsteroidal anti-inflammatory drugs (NSAIDs) and hormonal contraceptives to regulate or reduce menstrual flow. Dr. Jonnalagadda may also recommend lifestyle changes such as regular exercise and dietary modifications.
Endometriosis
● Overview: This condition involves the growth of uterine lining tissue outside the uterus. It can cause significant pain, especially during menstruation, and can affect fertility.
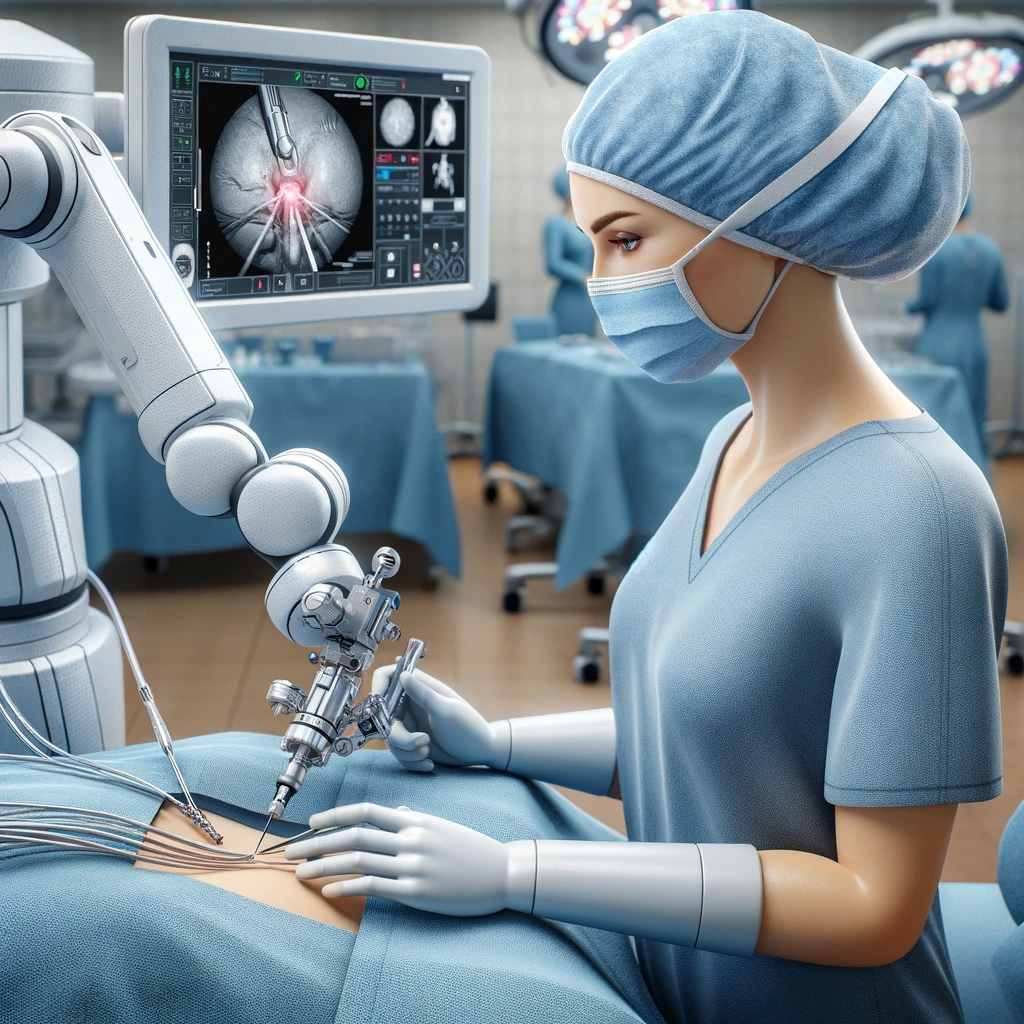
● Diagnosis and Treatment: Diagnosis may involve imaging tests like ultrasounds or MRIs, and in some cases, laparoscopy. Treatment options include hormonal therapies, pain relief medications, and in more severe cases, surgery to remove the endometrial tissue.
Ovarian Cysts
● Overview: Ovarian cysts are fluid-filled sacs that develop on the ovaries. While often asymptomatic, they can cause bloating, swelling, and sharp pain if they rupture.
● Monitoring and Management: Regular monitoring through ultrasounds is crucial. Most cysts resolve on their own, but if they become problematic, hormonal treatments or surgical options might be considered.
Fibroids
● Overview: Fibroids are benign tumors in the uterus that can cause heavy menstrual bleeding and a persistent sense of pelvic fullness or pain.
● Treatment Options: Treatment depends on the size and location of the fibroids and may include medication to regulate menstrual cycles and reduce bleeding, or minimally invasive surgical procedures.
Pelvic Inflammatory Disease (PID)
● Overview: PID is often a complication of sexually transmitted infections and can lead to severe pelvic pain and fever.
● Treatment: Early treatment is critical and usually involves a course of antibiotics. Dr. Jonnalagadda emphasizes the importance of early diagnosis and comprehensive treatment to prevent long-term complications.
Gastrointestinal Disorders
● Impact on Pelvic Pain: Conditions like irritable bowel syndrome (IBS) can cause symptoms that mimic or contribute to pelvic pain.
● Collaborative Care: In such cases, Dr. Jonnalagadda may collaborate with gastroenterologists to provide an integrated treatment approach.
Urinary Tract Infections (UTIs)
● Symptoms: UTIs can cause lower abdominal pain and discomfort during urination.
● Treatment: Typically involves a course of antibiotics, with a focus on prevention through lifestyle and dietary changes.
Diagnosing Pelvic Pain: A Comprehensive Approach
Dr. Jonnalagadda adopts a thorough approach that begins with an in-depth patient history and physical examination. Diagnostic tests may include ultrasounds, MRI or CT scans, laparoscopy, urinalysis, and blood tests. These help in pinpointing the exact cause of the pelvic pain.
Treatment Options: Tailored to Each Patient
Treatment plans at Advocare Montgomery Gynecology are personalized. They range from medications and physical therapy to minimally invasive surgery. Lifestyle modifications and alternative therapies are also considered to provide holistic care.
Dr. Jonnalagadda's Expert Approach to Pelvic Pain
Dr. Hema Jonnalagadda’s expertise in women's health is particularly evident in her approach to managing pelvic pain. At Advocare Montgomery Gynecology, she combines her deep understanding of gynecological health with a commitment to the latest medical advancements, ensuring that each patient receives the most effective, personalized care.
Personalized Treatment Plans
● Individual Assessment: Each patient’s experience with pelvic pain is unique. Dr. Jonnalagadda begins with a comprehensive evaluation, considering not just the physical symptoms but also the patient’s overall health, lifestyle, and emotional wellbeing.
● Collaborative Care: Recognizing that pelvic pain can have multiple causes, she works in concert with other specialists as needed, ensuring a holistic approach to treatment.
● Patient Involvement: Patients are active participants in their care. Dr. Jonnalagadda believes in empowering patients through education, helping them understand their condition and the treatment options available.

Utilizing Advanced Medical Technology
● Diagnostic Precision: Dr. Jonnalagadda employs state-of-the-art diagnostic tools, including advanced imaging and minimally invasive techniques, to accurately diagnose the cause of pelvic pain.
● Innovative Treatments: She stays abreast of the latest developments in gynecological treatment, offering patients access to the most advanced therapeutic options, from new pharmacological approaches to cutting-edge surgical techniques.
Emphasis on Comprehensive Care
● Addressing Emotional Wellbeing: Dr. Jonnalagadda and her team recognize that pelvic pain is not just a physical issue. They provide support for the emotional aspects of dealing with chronic pain, offering resources such as counseling and support groups.
● Long-term Management: Beyond treating immediate symptoms, she focuses on long-term management strategies to improve her patients' overall quality of life.
Conclusion: Compassionate Care for Pelvic Pain
The team at Advocare Montgomery Gynecology, led by Dr. Jonnalagadda, is dedicated to treating more than just the physical symptoms of pelvic pain. They aim to provide comprehensive care that addresses the full spectrum of a patient's needs, helping women find relief and improve their quality of life.
Call Us
If you're experiencing pelvic pain and seeking expert, compassionate care, reach out to Dr. Hema Jonnalagadda at Advocare Montgomery Gynecology.
Schedule an appointment today and embark on a journey toward better health and comfort. Dr. Jonnalagadda and her team are ready to provide the care and support you need to manage your pelvic pain effectively.